These links are provided for informational purposes only; they do not constitute an endorsement or an approval by SHINE.
Please contact us if you have a resource that could be shared on this page.

Related Websites/Networks
The World Health Organization (WHO) works with Member States to implement the tobacco control measures in the WHO Framework Convention on Tobacco Control (WHO FCTC), to reduce the prevalence of tobacco use and exposure to tobacco smoke.
The Smoke-Free Homes Network is a collaboration of researchers, healthcare practitioners and third sector partners in Scotland working to find innovative ways to reduce exposure to second-hand smoke in homes. You can learn more about network activities and aims here.
The Campaign for Tobacco-Free Kids and the Tobacco-Free Action Fund are the leading advocacy organizations working to reduce tobacco use and its deadly consequences in the United States and around the world. Through strategic communications and policy advocacy campaigns, they work to change public attitudes about tobacco and promote proven policies that are most effective at reducing tobacco use and save the most lives.
Action on Smoking and Health (ASH) Wales (UK) encourages households to adopt smoke-free home rules; provides guides, educational material.
Media campaigns and policy initiatives
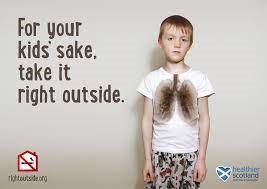
Take it Right Outside (TIRO)
The Scottish Government launched this national mass media initiative in 2014 encouraging smokers to smoke cigarettes outside their own home to protect children and other family members from second-hand smoke.
TIRO was accompanied by a world-first target aiming to reduce children’s exposure to second-hand smoke by 50% from 2012 levels by 2020. This target was achieved early in 2015 – with a reduction from 12% of children to 6% exposed to second-hand smoke. However, big inequalities still exist with much higher levels of child second-hand smoke exposure in poorer communities and no further reductions in the past 5 years.
You can access a range of TIRO videos on creating a smoke-free home, and car, and factsheets at nhsinform.scot

Resources for Parents
The Fresh Quit website includes several interactive resources for parents, relatives and carers. This includes practical information on how to protect children from second-hand smoke, facts about second-hand smoke, and information on the health risks of smoking in the car.

Training/Practitioner Resources
ASH Scotland has designed a trainer’s pack of activities and resources for early years practitioners who work directly with parent of young children. The pack is designed for use in parent sessions or parent classes rather than in a one-to-one setting.
The sessions cover the following key topics:
- Harmful chemicals in a cigarette and SHS
- What is SHS and how is it measured
- Health risks to children exposed to SHS
- Myths or misconceptions that parents/carers have about SHS
- Benefits to making a home smoke-free
- Challenges to making a home smoke-free and solutions to overcome these
- Action plan for making a home smoke-free
Please contact enquiries@ashscotland.org.uk for more information or to request a downloadable version of the full pack.
In addition, ASH Scotland has produced a pocket guide for discussing second-hand smoke with families, designed for family support workers.
Resources for Schools
NHS Greater Glasgow and Clyde developed its Jenny and the Bear story resource as part of a coordinated programme which aims to increase awareness about the effects of second hand smoke on children and what parents/carers can do to ensure their children are not exposed to its harmful effects.
The programme is aimed at Primary 1 classes and consists of a story being read to the class followed by a classroom activity to agree a name for the bear in the story, which is then entered into the competition to win a Teddy Bear mascot for their classroom. All children who take part in the programme will be given a booklet version of the story to take home.
Visit Jenny and the Bear for further details, and resources including a lesson plan and video.
Recent Publications
O’Donnell R, Howell R, Henderson T, et al. Use of nicotine replacement therapy to create a smoke-free home: study protocol for a pilot randomised controlled trial of a smoke-free home intervention in Scotland. BMJ Open 2025;15:e107161. https://doi.org/10.1136/bmjopen-2025-107161
O’Donnell R, Bintoro BS, Rustandi AW, Farahdilla ZA, Sadewa DMA, Padmawati RS, et al. COmmunities Facilitating incREasing Smoke-free Homes (CO-FRESH): co-developing a toolkit with local stakeholders in Indonesia and Malaysia. BMJ Global Health. 2025;10:e018102. https://doi.org/10.1136/bmjgh-2024-018102
Rodnay, M., Agbaria, N., Neumark, Y., Guri-Scherman, A. L. Y., & Bar Zeev, Y.(2024). “What can I do? fight him?”Perceptions and Experiences in Reducing Secondhand Smoke Exposure During Pregnancy: A Qualitative Study Among Israeli Women. Nicotine and Tobacco Research, ntae291 (2024). https://doi.org/10.1093/ntr/ntae291
Gupta A, Bansal A, et al. The crossroads of work and home: linkages between smoke-free policies at work and household environments. BMC Public Health 24, 1127 (2024). https://doi.org/10.1186/s12889-024-18658-9
Garritsen, Heike H., et al. “Associations of smoke‐free policies in multi‐unit housing with smoking behavior and second‐hand smoke exposure: A systematic review.” Addiction 120.4 (2025): 578-588. https://doi.org/10.1111/add.16724
Torosyan, Arevik, et al. “Facilitators and barriers to implementing smoke-free homes in Armenia: a qualitative study.” Global Health Promotion(2024): https://doi.org/10.1177/1757975925131872
Kamni SNA, Bahron NANBS et al. Knowledge, beliefs, perceptions and barriers related to implementing smoke-free home practices in two rural settlement areas in Malaysia. Tob Prev Cessat. Nov 22;10. (2024) https://doi.org/10.18332/tpc/195460
Tattan-Birch H, Jackson S et al. Are people more likely to vape or smoke indoors? a population survey of adults in England. Nicotine Tob Res 26;10 (2024): 1404-1411. https://doi.org/10.1093/ntr/ntae094
Guri-Scherman A-L Y, Neumark Y et al. Barriers and Enablers to Implementing a Smoke-free Home and Car During Pregnancy: A Qualitative Study Among Expectant Israeli Fathers, Nicotine Tob Res, 26;1 (2024) https://doi.org/10.1093/ntr/ntad149
Berg CJ, Haardörfer R, et al. “Examining local smoke-free coalitions in Armenia and Georgia: context and outcomes of a matched-pairs community-randomised controlled trial.” BMJ global health 9.2 (2024). https://doi.org/10.1136/bmjgh-2023-013282
Vijayaraghavan M, Hartman-Filson M, et al. Multi-level influences of smoke-free policies in subsidized housing: applying the COM-B model and neighborhood assessments to inform smoke-free policies.” Health Promotion Practice 26.1 (2025): 142-157. https://doi.org/10.1177/15248399231174925
O’Donnell R, Tigova O, et al. Supporting migrant groups to reduce tobacco-related harms and create smoke-free family environments: Future priorities and research gaps. Tob Induc Dis. 2024 Jun 13;22.
https://doi.org/10.18332/tid/189356
Hassanein, Zeinab M., et al. A qualitative study of barriers and motivators to prevent secondhand smoke exposure among pregnant women and children in Egypt: Identifying appropriate approaches for change.” Nicotine Tob Res 26;11 (2024). https://doi.org/10.1093/ntr/ntae051
Siddiqi K, Welch C, et al. “The effect of adult smoking behavior on children’s exposure to secondhand smoke. an analysis based on salivary cotinine levels among children in Dhaka and Karachi.” Nicotine Tob Res 26;11 (2024). https://doi.org/10.1093/ntr/ntae130
Sanz-Mas M, Continente X, et al. Changes in prevalence and socioeconomic inequalities in secondhand smoke exposure in Spanish children, 2016–2019. Tob Induc Dis. 22 (2024): 10-18332. https://doi.org/10.18332/tid/189392
Bidari M, Amrita G, et al. Changes in Prevalence of Childhood Exposure to Secondhand Smoke in India: A Secondary Analysis of GATS Survey (2009-2017).” Asian Pacific Journal of Cancer Prevention: APJCP 25.9 (2024): 3087. https://doi.org/10.31557/APJCP.2024.25.9.3087
Kibria, Md Golam, et al. “Assessing the choice of smoke-free policies for multiunit housing and its associated determinants in Bangladesh: a cross-sectional study.” BMJ Open 14.4 (2024): e074928. https://doi.org/10.1136/bmjopen-2023-074928
Chen T, Wang P, et al. “Increasing trends of household secondhand smoke exposure and widening socioeconomic disparities in Hong Kong adolescents, 2010–2020.” American Journal of Preventive Medicine 68;4 (2025): 735-744. https://doi.org/10.1016/j.amepre.2024.12.019
Talluri R, Shete S, et al. Secondhand tobacco smoke exposure in homes and vehicles in youth: disparities among racial, and sexual and gender minorities. Frontiers in Public Health 12 (2024): 1370552.
https://doi.org/10.3389/fpubh.2024.1370552
Possenti I, Gallus S, et al. Best practices for secondhand smoke and secondhand aerosol protection and evidence supporting the expansion of smoke-and aerosol-free environments: Recommendations from the 2nd Joint Action on Tobacco Control.Tob Prev Cessat 10 (2024): 10-18332.
https://doi.org/10.18332/tpc/193147
Mahabee-Gittens EM, Southworth H, et al. Assessment of the Smoke Free Families Tobacco Screening, Counseling, and Referral Program in Pediatric Primary Care Practices. Academic Pediatrics 24.2 (2024): 277-283. https://doi.org/10.1016/j.acap.2023.05.009
O’Donnell R, Dobson R, et al. Why should care workers be any different from prison workers? A qualitative study of second-hand smoke exposure during home-care visits and potential measures to eliminate exposure.” Ann Work Exposures and Health 68.9 (2024): 999-1003. https://doi.org/10.1093/annweh/wxae069
Perry EW, Self-Brown S et al. Evaluating the effectiveness of Smoke-Free Home SafeCare, an integrated intervention, among families at risk for secondhand smoke exposure and child maltreatment in the United
States: a study protocol for a hybrid type 1 trial. Trials 25.1 (2024): 661. https://doi.org/10.1186/s13063-024-08466-2
